Research Highlights
One step closer: ADK-L as a potential therapeutic target for aggressive metastatic breast cancer
Manipulation of the adenosine metabolite ADK-L may offer a way to modulate cell invasion and proliferation of breast cancer cells, offering a possible therapeutic solution to aggressive breast cancers.
Institution:
Legacy Research Institute, Mid-Columbia Medical Center
Team:
Bahar Shamloo*, Nandita Kumar, Randall H. Owen, Jesica Reemmer, John Ost, R. Serene Perkins, and Hai-Ying Shen*
Application:
3D culture for invasion assay
Disease model:
Breast cancer
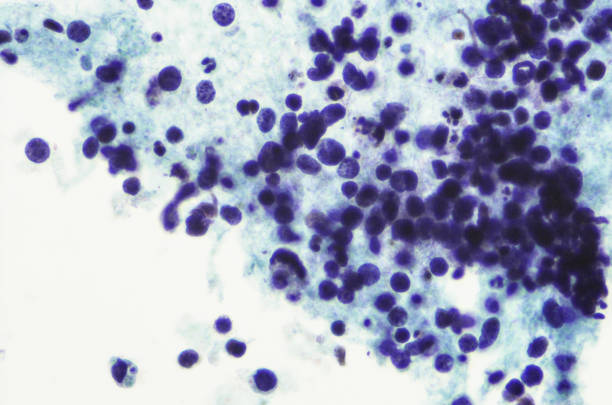
Cell types:
MDA-MB-231 (HTB-26), MCF7 (HTB-22), MCF 10A (CRL-10317)
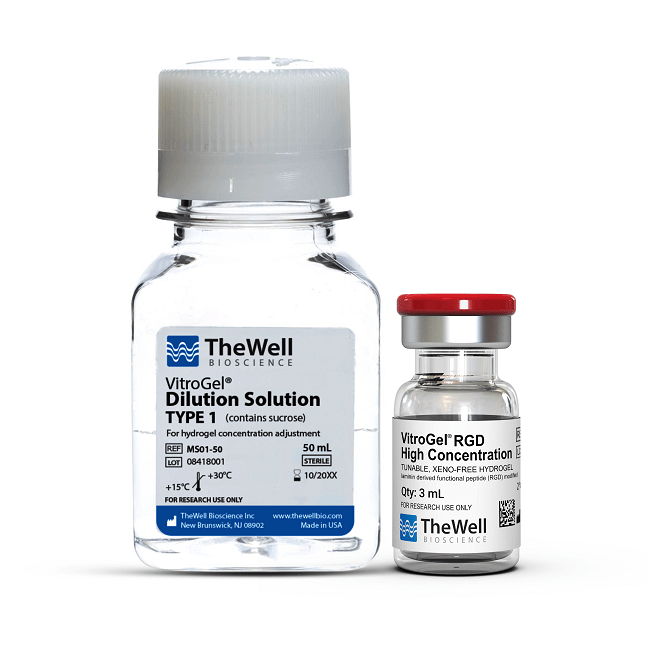
Hydrogel:
VitroGel® RGD (TWG003)
According to the American Cancer Society, breast cancer is one of the most prolific cancers in women in the United States, the second most common cause of death from cancer in women after skin cancer. While early detection is becoming more coming with routine screening practices, roughly 6% of women already have metastatic breast cancer upon diagnosis, however, the vast majority of cases result from early or mid-stage tumors that did not respond to available treatments. When breast cancer is detected before metastasis, the prognosis is excellent, with a 99% survival, however, for patients with metastatic breast cancer, the 5-year survival rate plunges to a mere twenty-seven percent. A major contributing factor for this is the lack of knowledge with regard to what allows for breast cancer metastasis, thereby making it difficult to pinpoint metastasizing or ready-to-metastasize cells.
A recent study by Bahar Shamloo and colleagues offers a possible solution. Citing previous studies that demonstrate that adenosine is critical in the regulation of several physiological functions including vasodilation, immune response, inflammation, all of which are critical for successful metastasis, they hypothesized that adenosine metabolism may be a driving force in breast tumor metastasis. To investigate this, they evaluated both isoforms that result from adenosine deamination, ADK-S, and ADK-L, for their ability to modulate breast cancer cells both molecularly and physiologically. They found that in several types of breast cancer tissues, ADK-L, but not ADK-S was upregulated compared to adjacent non-cancerous tissue samples and that CRISPR-mediated knockdown of both ADK isoforms reduced the proliferative capacity and cell viability, demonstrating a significant reduction in genes that drive these physiological responses. Most notably, they observed that disruption of ADK-L expression disrupted the invasive capacity of these cells. Using TheWell Bioscience’s VitroGel RGD tunable hydrogel scaffold to mimic the extracellular matrix, they evaluated the ability of unmodified breast cancer tissue and ADK-L-null breast cancer tissue to invade through the hydrogel extracellular membrane and a microporous scaffold mimicking the basement membrane to get through to nutrient media below. Though results for different types of breast cancer tissues varied, they noted a downward trend in the ability of cells to invade the hydrogel and microporous scaffold, suggesting that manipulation of this specific metabolite can be used to control breast tumor cells and may be the key to developing better methods of treatment and diagnosis of metastatic cancer and perhaps facilitate the identification of some types of pre-metastatic breast tissue. Interestingly, while the authors note that results vary in different types of cancer tissues following manipulation of ADK-L, they had the most remarkable success with cells derived from the most aggressive of the cancer lines tested: receptor triple-negative breast cancer tissue. Though further studies are necessary to understand this mechanism by which gene manipulation rendered the physiological outcomes and to evaluate extraneous effects of gene modification, this study offers a promising new avenue for developing targeted therapeutics for aggressive metastatic breast cancer.
Multiple previous studies have demonstrated the importance of accurately mimicking the 3D microenvironment in order to properly develop cancer therapeutics and detection methods. VitroGel is a tunable peptide hydrogel that can accurately assemble into a scaffold that recapitulates the extracellular matrix. In order to spread, cancer cells must break through several membranous structures starting with the tumor capsule (regional metastasis) and ultimately gaining access to the circulatory or lymphatic system (systemic cancer) in order to ultimately progress to stage four, therefore necessitating a precise, modifiable means by which to model and study cancer cell invasion. The inherent flexibility of the VitroGel hydrogel scaffold can facilitate this model.
Related Product: