Research Highlights
Getting to the root of the problem: Injectable VitroGel® 3D hydrogel scaffolds enhance odontogenic differentiation in vivo
The biocompatible and injectable VitroGel hydrogel culture system enhances pulp-dentin regeneration and has the potential for chair-side regenerative endodontic procedures
Institution:
The Fourth Military Medical University, China Medical University
Team:
Min Xiao, Jun Qiu, Rong Kuang, Beidi Zhang, Wei Wang*, Qing Yu *
Application:
In vivo utilization to study biocompatibility and differentiation potential of primary human apical papilla stem cells.
Disease model:
Apical periodontitis
Cell types:
Apical papilla
Hydrogel:
VitroGel® 3D (TWG001)
Regenerative endodontic procedures are common for repairing immature permanent teeth with apical periodontitis. These procedures are commonly successful and result in stabilization of proper successful root development of previously contaminated teeth. However, for teeth exhibiting apical periodontitis with pulp necrosis, current regenerative options present issues with proper revascularization and compromised root development, leading to substantial risk for root fracture.
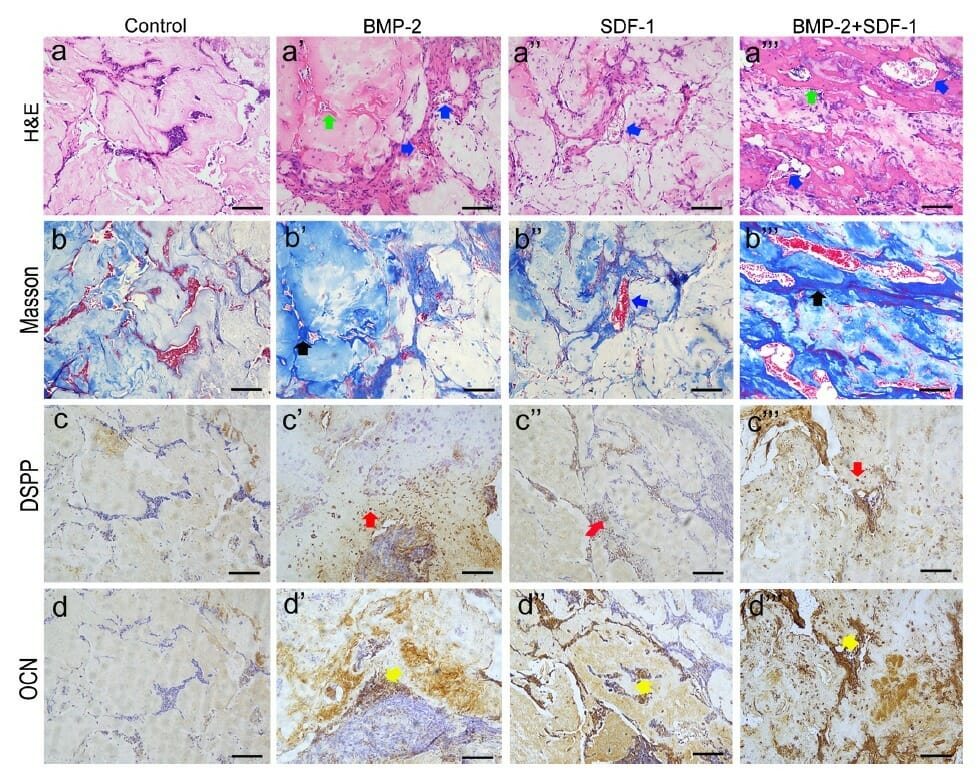
A recent study sought to address this. Using TheWell Biosciences’ injectable VitroGel® 3D tunable hydrogel, Min Xiao and colleagues tested the biocompatibility and differentiation potential of primary human apical papilla stem cells. To do this, they isolated healthy apical papilla stem cells from molars of healthy individuals, expanded them ex-vivo, and seeded them in the hydrogel. Preliminary studies noted no difference in proliferation between 2D and 3D cultures and high cell survival, indicating high biocompatibility. Xiao was also able to show that in vitro exposure of hydrogel-encapsulated cells to BMP-2 and SDF-1a, two factors individually shown to efficiently promote odontoblast differentiation, caused cells to express the early odontoblast marker DMP-1 and later marker of mineralized bone, OCN. Interestingly, these two factors worked synergistically, inducing more differentiation together than either factor working along. Finally, and most impressively, Xiao and colleagues were able to use the injectable feature of VitroGel 3D to demonstrate that the apical papilla-seeded hydrogel inserted into subcutaneous pockets of nude mice were able to able to generate vascularized fibrous connective tissues, something current treatments for degenerative pulp-dentin conditions have failed to do! Because VitroGel 3D is compatible with various histochemical assays, detailed molecular analysis of the specimens could be performed, revealing that the hydrogel encapsulated samples treated with both BMP-2 and SDF-1a produced the most osteoid dentin and secreted the most collagen matrix of all the samples. Moreover, semi-quantification of the vessels via CD-31 endothelial cell staining showed twice as many vessels as other samples. Finally, they were able to show that the growth of apical papilla cells in VitroGel 3D was able to promote hard tissue regeneration in vivo, a necessary phenotype for proper root development.
Choosing an ideal scaffold is very important for odonatological applications; should be biodegradable and able to facilitate cellular infiltration, vascularization, cell differentiation and eventual replacement by the appropriate tissues, and must settle easily into small, inconsistent spaces. To this effect, injectable scaffolds have become popular; however, thus far, none have been ideal for fast-paced clinical practice. Moreover, each presents different problems from the production of degradation byproducts to the lack of biomimetic surface structures that can interact with endogenous cells, to the inability to biodegrade. TheWell Bioscience’s VitroGel3D is stable at room temperature, has a neutral pH, and is ready for injection with cells/compounds, making it an ideal scaffold for clinical approaches. It is tunable, injectable, and highly biocompatible for use in a variety of applications. Though Xiao’s in vivo results thus far are only subcutaneous, these preliminary studies have revealed VitroGel system as a promising candidate for future research on tooth root regeneration, providing a platform that can easily bridge in vitro molecular studies and in vivo clinical studies, and can get to the root of the problem for tooth root regeneration!
Related Product:


