Research Highlights
Mice Recruited to Help Fight Cancer of the Thymus
Institutions:
Gifu Graduate School of Medicine, Japan
Team:
Niwa, R., Hanamatsu Y., Kito, Y., Saigo, C., and Takeuchi, T.
Disease Model:
Thymic Cancer
Hydrogel:
VitroGel® Hydrogel Matrix
A mouse model of thymic cancer is described, and the results show that viral infection may not always be the cause.
In this paper, a team of oncologists from Japan sought to elucidate some of the key events that occur in the thymus, an important organ in the immune system, as a tumor forms. They studied a rare subtype of thymic neoplasm called micronodular thymic neoplasm with lymphoid stroma (MNT). In this cancer, the triggers and pathways to tumor formation are poorly understood, warranting a more thorough analysis.
The authors used a mouse model to pursue a better comprehension of tumorigenesis in MNT. They extracted a thymic tumor from an immunodeficient mouse and analyzed it using several histochemical markers. Then they grew these cells in an ex vivo three-dimensional cell culture, allowing further immunochemical and histochemical analyses. A critical aspect of their study was that they could then transplant these cancerous cells into BALB/c mice. This allows for precisely tracking how existing tumor cells stimulate further tumor formation. To enhance the quality of their cell transplantation in this regard, the authors mixed their cultured cells with TheWell Bioscience’s VitroGel® Hydrogel Matrix before cutaneous injection. This xeno-free matrix helps promote a suitable environment for both injection and later successful cell grafting. After implantation and growth for two weeks, the tumors were then removed for histopathological studies.
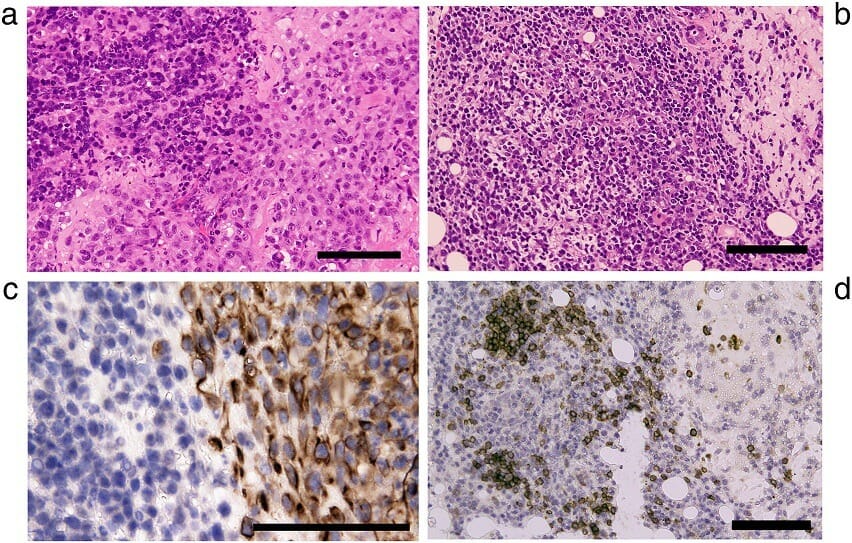
The authors noted several important trends throughout these studies of thymic tumor properties and expression of cell surface markers. First, the original thymic tumors from mice that they examined exhibited multiple polygonal “cell nests” having lymphoid stroma, a property that is shared by human thymic tumors. These nests displayed the immunochemical staining reactivity that is characteristic of epithelial cells. Second, more specifically, the cultured tumor cells exhibited surface cell markers CD3, CD4, and CD8 indicative of various types of T cells that represent particular stages of thymic differentiation (i.e., tumor formation). And thirdly, upon transplantation into cancer-free mice, the cells grew into tumors akin to human thymic tumors from histological and pathological points of view.
From these data, the authors concluded that epithelial cells play a critical role in the advancement of thymic tumors. This conclusion perhaps dispels a common hypothesis that Epstein-Barr viral infections are a causative agent in thymic tumor formation, at least in the case of MNT. In any event, the authors have described a useful mouse model for the study of how human cancers of the thymus develop and can be fought.