Research Highlights
Characterization of Lipopolysaccharide-Induced Prostate Cancer Formation and Possible Amelioration of This Process by the Antibiotic Trichostatin A
Institution:
Affiliated Aoyang Hospital of Jiangsu University, Zhangjiagang, China
Team:
Tang S., Lian X., Cheng H., Guo J., Ni D., Huang C., Gu X., Meng H., Jiang J., and Li, X.
Application:
Establishment of a tissue-mimicking 3D cell culture to test tumor formation, progression, and inhibition in prostate cell lines.
Disease Model:
Prostate Cancer
Hydrogel:
VitroGel® RGD
The progression of tumorigenesis during prostate cancer is often accompanied by bacterial infections, which can exacerbate and accelerate the transformation of epithelial cells to mesenchymal cells (the EMT). The exact mechanism by which this bacterial stimulation of cancer cell formation is not known, but it is thought to be mediated by the interaction of the lipopolysaccharide (LPS) on the outer membrane of the bacterial with membrane proteins of prostate cancer (PCa) cells. The transformation can then occur by EMT-related signaling pathways, including the Stat3 pathway. The characteristic of EMT that can be quantified is the “stemness,” which is the morphological state of PCa cells that indicate a regression to a stem-like tumorosphere. The authors of this study sought to examine and quantify the degree of LPS-induced EMT and stem-like cell formation in a variety of PCa cell lines. With such information, it might be possible to explore the efficacy of a particular antifungal/antibiotic Trichostatin A (TSA) in slowing tumor progression.
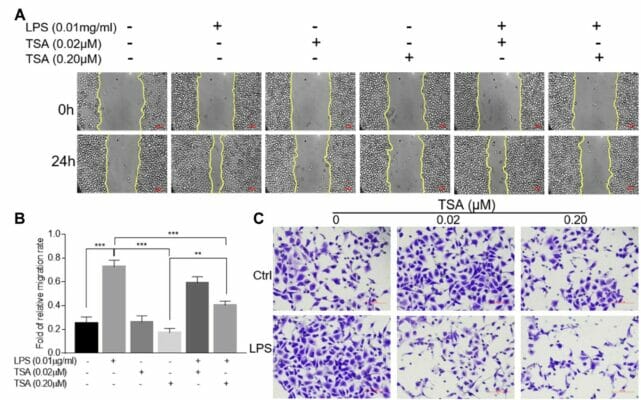
The authors tracked the growth of normal prostate cell lines in culture and their response to wounding, invasion, tumor formation, and how these events differed in varying concentrations of TSA and/or LPS. Measurement of cell morphology and stem-ness was performed by fluorescence microscopy and flow cytometry. Importantly, the cell cultures were maintained in a three-dimensional environment by the use of VitroGel RGD. In this technique, the tumorospheres were collected and mixed with VitroGel RGD such that a hydrogel was formed. The cover medium was changed every two days, allowing sustained growth. At predetermined times, the hydrogel was fixed and stained such that microscopy was possible. The results of the study were that LPS stimulated cell invasion, self-renewal, and transformation. This bacterial macromolecule significantly (at the P < 0.001 level) induced PCA epithelial cells to undergo EMT and enhance their stem-ness. On the other hand, dosing the cells with 20 nM TSA following treatment with 0.01 mg/ml LPS revealed that the antibiotic could retard tumor cell number and migration in a dose-dependent fashion. TSA appears to exert its effects through the inhibition of Stat3 phosphorylation and c-Myc expression, and thus interferes with the cell-signaling pathways that are directly involved in tumor formation.
Read the publication:
Related Products: