Research Highlights
Long-Lived Lab Grown Cells for Diabetes Treatment
Institutions:
City of Hope National Medical Center, CA
Team:
Omori, K., Qi, M., Salgado, M., et al., and Kandeel, F.
Disease Model:
Diabetes & Kidney Transplantation
Hydrogel:
VitroGel® 3D
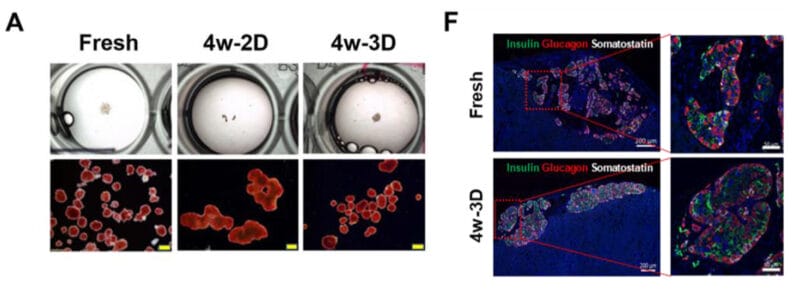
Human islet beta cells can be grown in 3D cell culture for up to eight weeks, rather than the three days they would survive in standard 2D culture. These cells retain their potency to deliver insulin both before and after transplantation.
Human islet β cells are found in the pancreas and secrete insulin to regulate blood sugar levels. For those with Type 1 diabetes (T1D) however, these cells are diminished and cannot produce insulin at the required rate. Thus, one therapy available for treatment of severe T1D is islet cell transplantation from a healthy donor, sometimes accompanied by kidney transplantation to help stave off renal failure. Unfortunately, islets can only survive about three days in standard (2D) cell culture. Thus, there is recent excitement surrounding the concept of using 3D cell cultures to prolong the longevity of islets in the lab, because these conditions more naturally mimic the organoid structure of islets in the native physiological state.
In this new publication, a team of cell biologists from the City of Hope Research Institute in Duarte California sought to demonstrate that islets can be sustained over the long term in 3D hydrogel-based cell culture media. The investigators embedded human islets in TheWell Biosciences’ VitroGel 3D and attempted to maintain the cells alive for weeks, rather than days. The 3D culture medium was xeno-free CMRL 1066-media with the CIT (Clinical Islet Transplant Consortium) modifications with added IGF-1 heparin, and human serum albumin. The cells were grown at 37 °C in room air with 5% added CO2 for 2, 4, or 8 weeks and then assayed for in vitro and in vivo characteristics. For comparison, the cells were also grown in standard 2D culture medial.
The team examined the masses of islets that could be recovered under each condition, along with their viability, purity, ability to secrete insulin, gene expression levels, and propensity to be transplanted into live diabetic SCID mice. In short, they found that VitroGel 3D could maintain human islet mass, viability, and function for as long as eight weeks. The cells grown under these conditions also exhibited mRNA-assayed gene expression levels for key pancreatic function markers that were not statistically distinct from fresh islets. Importantly, the team demonstrated that the culture system could be scaled up from the 150 μL test conditions (under which these assays were made) to a much larger 2.5 mL volume with no loss of relative insulin production. Finally, the City of Hope team injected islets from the scaled-up system into diabetic mice and found that they could reverse the symptoms of diabetes, specifically they could normalize the mice’s blood glucose levels. The transplanted cells could express insulin, glucagon, and somatostatin proteins at normal levels.
In conclusion, this research study was very successful at showing that human islets could be maintained for many weeks in 3D cell culture with no degradation of function. These cells can be cultured in a relatively large scale and transplanted into live subjects, reversing diabetic phenotypes. This paper offers great hope for an additional powerful therapeutic tool in the treatment of both Type 1 and Type 2 diabetes.


